Hypermobility; What Does it Mean if Your Joints are too Flexibile?
Posted by Phil Heler on June 27, 2023Excessive movement is not as unusual as you would think. Hypermobility affects approximately 20% of the population. The most common thread for many of these people is a genetic disorder that influences how their bodies make collagen which is the main structural protein that we are made of.
As you would expect most of my work comprises helping people with problems that relate to movement. Usually, a lack of it. This can manifest for a host of reasons that we are all too familiar with. These range from the incessant march of time and its effects on our body, our own unrealistic ambitions as we lift something that we shouldn’t, or just a simple slip or fall.
Depending on the anatomy book you reference our bodies have roughly 496 joints, 372 of which are moveable and 173 of these are associated with the ribs and spine. All this connected by 206 bones. Obviously, soft tissue related complaints could potentially involve any of the 650 or so named muscles that exist in our body and their respective tendons. Throw 900 ligaments in the mix and there is a lot that can go wrong!
One of my most difficult conundrums is what to do when someone says they have too much movement (or hypermobility) when my aim is to typically stretch, move and mobilise a tissue of one sort or another. Excessive movement is not as unusual as you would think. Hypermobility affects approximately 20% of the population. Many of these people will be able to touch their thumb to their inner forearm or place their hands flat on the floor without bending their knees (what we sometimes call ‘double-jointed’). The most common thread for many of these people is a genetic disorder that influences how their bodies make collagen which is the main structural protein that we are made of.
One way to measure joint hypermobility is a general screening protocol called the Beighton Scoring System which measures joint hypermobility in your fingers, elbows, knees and spine using a 9-point scale. One point is given for each of the following joints that shows hypermobility as seen below.
Whilst the Beighton score is a good general screening tool it does have a few glaring omissions. Key joints such as the jaw, neck, shoulders, ankles, feet or toes are not factored into the index. Clearly sometimes relying on the Beighton score is not enough. If a person has joint hypermobility in a myriad of different areas this may not be factored into the assessment.
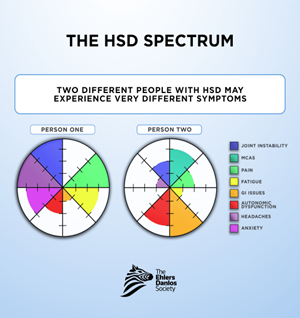
Unfortunately, hypermobility does not just end with the bony and soft tissue structures (the musculoskeletal system). As a condition it is much more profound than just a series of overly flexible joints. Hypermobility is considered as being on a spectrum. This is because symptoms vary widely both in their type and severity, even between two different people. This spectrum of symptoms involves our entire body rather than specifically those components that enable movement.
Collagen is pervasive throughout our anatomy and makes up one third of the total amount of protein inside us. Unbelievably there are 28 different types of collagen, each of which has a specific role to play. Combined, all these classes of collagen help make up our skin, tendons, blood vessels, cartilage, bone and connective tissue. For the sake of definition connective tissue is composed of what is known as extracellular matrix. This is a network of molecules that holds our body’s tissues in place. As such collagen is essential for everything from joint health, protection of our internal organs, skin elasticity, a healthy cardiovascular and gastrointestinal system and even the structural integrity of our bone.
Based on this, as you can imagine, people with hypermobility spectrum disorders (or HSD) can suffer from a wide variety of symptoms. Collagen disorders have the potential to affect our cardiovascular system (our four heart valves are made of collagen, as is our vascular system) or gastrointestinal systems (your stomach has two valves or sphincters).
There is also increasing evidence that HSD symptoms can be associated with widespread general systemic symptoms. These include fatigue, anxiety, headaches and autonomic dysfunction. The autonomic system (ANS) governs our internal systemic balance regulation. There is another condition which is called Mast Cell Activation Syndrome (or MCAS). This is another lesser-known condition associated with hypermobility which leads to a wide range of issues such as fainting, nausea, headaches, fibromyalgia and variable blood pressure.
As we mentioned HSD is termed as such because two people will experience very different symptoms as defined below. For example, one person with HSD may have joint instability, fatigue, and autonomic dysfunction. Another person with HSD may have mild joint instability but also severe headaches and gastrointestinal issues. Both people will be affected by HSD uniquely, but neither person has “more HSD” than the other. All of this boils down to your genetic makeup.
The 28 different collagen types are made and encoded by 43 different genes (we have approximately 20,000 genes in all). Even our genes can have faults (or mutations). There are at least 70 distinct types of known gene mutations affecting two of the most important of these 43 genes. COL1A1 and COL1A2 express the most common form of collagen called type 1. It is a key constituent in tendons, skin, bones and ligaments. For the purposes of this article, I am focusing on the key condition generated by mutations affecting COL1A1 and COL1A2. This key condition is known as Ehlers-Danlos Syndrome.
Mention hypermobility in my profession and most people will, in the same breath, say Ehlers-Danlos Syndrome. Although hypermobility in general had been known about for a long time it was not until 1901 that it was described by Lauritz-Edvard Ehlers of Denmark who presented his findings at a conference. The syndrome was again described in 1908, this time by a French doctor named Henri-Alexandre Danlos. Now we have a name. The key observations that our Danish and French scientists focused on was hypermobility and skin stretch.
Since then, it has been realised that Ehlers-Danlos syndrome (or EDS) is a group of 13 inheritable collagen disorders that affect COL1A1 and COL1A2 that synthesise type 1 collagen. As genetic markers continue to be discovered this may increase. Each type has its own set of features (although some are seen across all types of EDS), each with its own set of diagnostic criteria. Each of these variations of EDS have a different prevalence in the general population. The most common form is Hypermobile EDS and accounts for about 90% of all EDS that is diagnosed. It is estimated to affect at least 1 in 5,000 people. The reality is that it is probably much more common and may be underestimated despite being categorised as a rare disease.
Other forms of EDS really are quite rare. These include Classical EDS (1 in 20,00-40,000) and vascular EDS (1in 100,000-200,000). All other types of EDS are classified as ultra-rare, affecting less than 1 in 1 million people. Several types of EDS have only been reported in a few affected families.
There is no specific treatment for EDS but it is possible to manage the symptoms with support and advice. Key considerations are strengthening joints and avoiding stressful activities that may compromise joint stability, which is where I help. I can also recommend supports for various joints which are the most flexible and liable to injury because of their hyperflexibility. Genetic counselling can help people understand their condition and inform on the likelihood of inheritance. Clearly for those people who are affected by cardiovascular or gastrointestinal related symptoms, diagnostic imaging can help identify key issues.