About 20% of sports injuries involve the shoulder. Shoulder injuries are most common in sports that involve overhead movement, like tennis, cricket, swimming, weightlifting and volleyball.

The most common shoulder injuries are rotator cuff injuries, shoulder impingement and shoulder dislocation/instability.
Shoulder injuries – rotator cuff
Typical symptoms: General shoulder pain that increases with raising your arm or even sleeping on the affected shoulder.
Rotator cuff tears in the shoulder are a common issue in any sport that involves throwing, pushing, pulling or lifting. The humerus (upper arm bone) has a rounded head that forms a ball and socket joint with the scapula (or shoulder blade).
An analogy would be like a golf ball sitting on a shallow tee, this allows great natural movement with the trade-off being stability.

The rotator cuff solves this dilemma as it makes a network of four muscles whose tendons coalesce to cover the head of the humerus, therefore serving to ‘strap the golf ball on the tee’. The rotator cuff muscles consist of the supraspinatus (runs across the top of the head of the humerus) and the subscapularis (which runs across the front) and the infraspinatus and teres minor muscles (which run across the back). These muscles are also very important in rotating or lifting your arm.
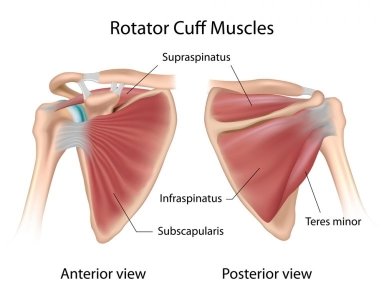
If you have suffered an injury to your rotator cuff, you may experience pain or weakness when lifting your arm. The pain is usually over the deltoid region (on the outside of your upper arm). Typically, rotator cuff injuries may cause difficulty with basic functional tasks like lifting, reaching, or sleeping.
Problems start when one or more of these tendons (most often the supraspinatus) are damaged or torn completely (full thickness tear) and no longer attach to the head of the humerus. Most often this is seen in the dominant shoulder and can be the result of repetitive stress motions seen in sports such as tennis, rowing or cricket, or falling on an outstretched arm. Blood supply to the rotator cuff tendons does also diminish with age and this can impair healing. With age we can also develop bony spurs in the shoulder that rub on the rotator cuff tendons and the tendons themselves can become calcified due to longstanding inflammation.
Typical symptoms start with an acute onset of pain, particularly on any movement of the shoulder (especially overhead movements). Treatment involves analgesia and anti-inflammatory medications (under advice from your GP), physical therapy and rehabilitation in order to maintain strength and flexibility. Cortisone injections can help reduce pain and inflammation, although repeated injections may serve to further weaken the tendon. If the shoulder does not improve and there is a larger or complete tear, surgery may be the best option to reattach or repair the tendon.
Shoulder injuries – impingement syndrome
Typical symptoms: General shoulder pain more commonly as we age. Gradual onset, increased pain when active or at rest and sleeping on the affected shoulder.
Impingement syndrome occurs in people who engage in physical activities that require repeated overhead arm movements, such as tennis, golf, swimming, weightlifting, or throwing a ball. Occupations that require repeated overhead lifting or work at or above shoulder height are also at risk.
Rotator cuff tendons are protected as they pass into the shoulder by bones (mainly the acromion) and ligaments that form a protective arch. As the tendons pass through the arch there is a protective lubricating sack called a bursa (subaromial bursa) that forms a smooth friction-free surface to allow the tendons to slide over one another and avoid rubbing on bony surfaces. The main bone that forms the protective arch (the acromium) can develop bony spurs as we grow older. This is illustrated in the diagram below. This narrows the space and can rub on either the rotator cuff tendons or bursa resulting in tendinopathy or bursitis.

Shoulder dislocation and instability
Traumatic shoulder dislocations are most common. The shoulder tends to dislocate forwards and down in 96% of cases (this is known as an anterior dislocation and is illustrated below). This is usually associated with a sports-related injury in young people or falling with an outstretched arm for older people. Other types of dislocations which are rare are is when the shoulder is displayed backwards (4%) or downwards (one in 200 cases).

Some people are also inherently more mobile than others. This occurs for various different reasons. Some of us are just naturally hypermobile. In fact there is a scoring system based on hypermobility called Beighton’s Hypermobility Index that uses a 9-point index for joint laxity, with 6 points or more being an indicator of hypermobility. In such cases we often see multi-directional instability, with the head of the humerus being unstable in all directions, and this is obviously allied with a capacity to dislocate. These people are often what we term as ‘double jointed’.
Other people can also have joint laxity because of repetitive overhead movements that are typical in many sports such as cricket, swimming and tennis or in jobs which require regular and repetitive overhead motions. Once the ligaments, tendons, and muscles around the shoulder become loose or torn, dislocations can occur repeatedly. Chronic shoulder instability is the persistent inability of these tissues to keep the arm centred in the shoulder socket.
Shoulder instability is therefore often classified into two large groups by orthopaedic surgeons:
TUBS stands for:
-
Traumatic
-
Unilateral (i.e. one shoulder)
-
Bankart and Hill-Sachs lesions (bony injuries)
-
Surgery
AMBRI stands for:
-
Atraumatic (no trauma)
-
Multi-directional (loose in different movements)
-
Bilateral (both shoulders affected)
-
Rehabilitation (generally responds well to rehab)
-
Inferior capsular shift (if rehab fails)
This model is quite simplistic and surgeons now often use the Stanmore Triangle which classifies a third group of patients that have recurrent dislocations because of loss of shoulder integrity.