Coronavirus COVID-19: Self-Hygiene
Posted by Phil Heler on March 6, 2020Coronavirus COVID-19 infection: how it compares with flu and the role of self-hygiene.
Coronavirus COVID-19 has arrived on our doorstep and rates of infection are increasing. UK health officials are moving towards the second phase of their response to the coronavirus outbreak. It comes as the number of UK people diagnosed with the virus reached 115, a rise of 30 since Wednesday. At our clinic we are now undertaking a deep clean every morning before start of business and we have hand sanitisers stationed on point of entry to the clinic. We also insist that people use the provided hand sanitisers after leaving our treatment rooms. This is for your safety and ours! It would be wise consider a similar hand washing routine at home. This will help prevent community spread.
There are two kinds of response to a growing pandemic. The first is containment: as cases appear, you can isolate each person then trace and quarantine their contacts. This having been policy the UK and abroad. This worked well for SARS for instance. The second is mitigation. Eventually you get “community spread”: people are infected without knowing how they were exposed, so it is impossible to quarantine all contacts. You close schools, cancel mass gatherings – or as China did, and Italy is now doing, shut down whole cities when they have community spread. This will stop an epidemic peaking at rates that will not overload health facilities and other aspects of infrastructure. We are not currently at this stage in the UK. But we have learned from what has happened in China.
How Does Coronavirus COVID-19 Compare with Flu?
The Chinese Centre for Disease Control and Protection (China CDC) has undertaken the largest study on Coronavirus COVID-19 cases. They analysed 44,672 confirmed cases in China between December 31st, 2019 and 9th February 2020. Of those cases, 80.9% (or 36,160 cases) were considered mild, 13.8% (6,168 cases) severe and 4.7% (2,087) critical. What is important to remember is that the mortality rate for COVID-19 appears to vary by location and an individual’s age, among other factors. For instance, in Hubei Province, the epicentre of the outbreak, the mortality rate reached 2.9%; in other provinces of China, that rate was just 0.4%, according to the China CDC. In terms of age the mortality rate soars to 14.8% in those 80 and older; among those ages 70 to 79, the Coronavirus COVID-19 death rate in China seems to be about 8%; it’s 3.6% for those ages 60 to 69; 1.3% for 50 to 59; 0.4% for the age group 40 to 49; and just 0.2% for people ages 10 to 39. No deaths in children under 9 have been reported.
So far, the new coronavirus COVID-19 has led to more than 89,000 illnesses and 3,000 deaths worldwide. How does that compare with flu? This is a very common question. In the U.S. alone, this flu season so far, minimum estimates suggest that there has been an estimated 32 million illnesses (U.S population is 327 million), 310,000 hospitalisations (0.97%) and 18,000 deaths (0.06%) according to the U.S Centres for Disease Control and Prevention (CDC). Currently there is no data available in order to ascertain mortality rates for different age groups for this season. However, there is for 2018-19 when there were 35.5 million estimated flu related illnesses in the U.S.
Estimates of hospitalisations and mortality associated with the 2018–2019 flu season demonstrate 490,600 hospitalisations (1.4%) and 34,200 deaths (0.09%). In other words, 98.5% cases did not involve medical attention. More than 46,000 (9.4%) hospitalizations occurred in children (aged <18 years); however, 57% of hospitalisations occurred in older adults aged ≥65 years. Older adults also accounted for 75% (or 25,650 in total or 0.07% of total cases) of influenza-associated deaths, highlighting that older adults are also vulnerable to flu infection. The important thing to remember as well is that there is a much higher chance of coronavirus COVID-19 leading to serious respiratory symptoms than seasonal flu.
Sneezing & Coughing & Face Masks
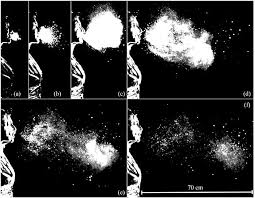
The Massachusetts Institute of Technology in 2014 looked at how far coughs and sneezes travel, and the results were surprising. Coughing spreads droplets as far as six metres and sneezing as much as eight metres! Some studies suggest that an average sneeze or cough can contain 100,000 contagious viral particles and delivered this load at speeds up to 60-100 miles per hour. Uck!
One of the key vectors of transmission for coronavirus COVID-19 is sneezing and coughing. Clearly any respiratory tract infection gives us the compulsive reflex to cough or sneeze. Coughing helps clear the airways of mucus and remove excess fluids from the lungs, especially when normal mechanisms of clearance are overloaded or impaired. During a cough or sneeze, droplets of airway secretions become airborne. Once expelled from the mouth in a high velocity sneeze these secretions or droplets from what researchers charmingly call a “multiphase turbulent buoyant cloud”! The aerosol droplets generated during coughing or sneezing span a broad size range, from mere nanometres (this is a billionth of a metre) to hundreds of micrometres (one millionth of a metre). The dispersion of these droplets in the environment depends to a large extent on just how big they are. Most of the larger, heavier drops fall quickly to the floor or on other hard surfaces under the influence of gravity. Obviously good self-hygiene is very useful at this point. If you sneeze into a tissue, this doesn’t happen in the first place.
Given that we may accidentally walk into one of these “multiphase turbulent buoyant clouds” does it make a difference if we wear a face mask? Unfortunately wearing a face mask is not an iron clad guarantee. Firstly, this is because smaller droplets in aerosols can still penetrate masks and it is important to remember that a virus can also transmit through the nice moist tissue in your eye. The Centres for Disease Control and Prevention (CDC) in the U.S. state that you should only wear a mask if you yourself are infected with the new coronavirus or if you are taking care of someone who may be infected. If you’re just walking around town and not in close contact with others, wearing a mask is unlikely to make any difference.
How Long is Coronavirus COVID-19 Dangerous for on Different Surfaces?
A study performed in 2011 at Public Health England (PHE) suggest that after nine hours, viruses are no longer viable on hard non-porous metal and plastic surfaces, such as aluminium and computer keyboards. On porous items, like soft toys, clothes and wooden surfaces, viable viruses disappear after four only hours. Because most viruses don’t often last beyond nine hours (even on a hard surface) research suggests public spaces like classrooms, offices and kitchens that are not populated at night will usually be free of contagious flu viruses the next morning. We are much more proactive at our clinic. We are now sanitising all hard surfaces as floors, desks, desktop equipment such as keyboards, even door handles and the keypad on our credit card machine!
The best surface for killing viruses is surprisingly our skin. In the cases of both flu and cold-causing viruses, infectious particles on our skin last no longer than 20 minutes. Between its pH and its porous nature, our body’s natural barrier does a great job at killing viruses. Our hands are also a common vector of transmission even if there is only a 20-minute window. We as individuals typically touch our faces an average of 15 times per hour. Bearing in mind that our hands are in frequent contact with all forms of hard surfaces from door handles to keypads, petrol pumps and currency. We may subsequently contact our mouths or rub our eyes, each being entry point for a virus. Therefore, hand washing is critical.